phlebeurismis a pathological condition characterized by a change in the structure of the venous system, which leads to an increase in the diameter of the lumen of the superficial veins and a disturbance of the valve system, which manifests itself in valve failure, i. e. in its incomplete closure of the vein.
Normally, blood flows through the veins against the force of gravity, from bottom to top, which is possible only thanks to the work of venous valves. Under the influence of various reasons, primary (due to changes in the valve itself) or secondary (due to dilation of the vein) valve failure occurs; This condition is characterized by incomplete closure of the venous valve and reverse blood flow. The reverse flow of blood aggravates the changes in the venous wall and also contributes to blood stagnation in the lower extremities, causing swelling of the lower extremities and a feeling of heaviness in the legs.
In addition to stagnation of blood in the lower extremities, the above processes lead to a disruption of linear blood flow through the veins from top to bottom, the appearance of reflux (reverse blood flow) and turbulent blood flows in the expansion area . Changes in blood flow characteristics are the main cause of thrombosis.
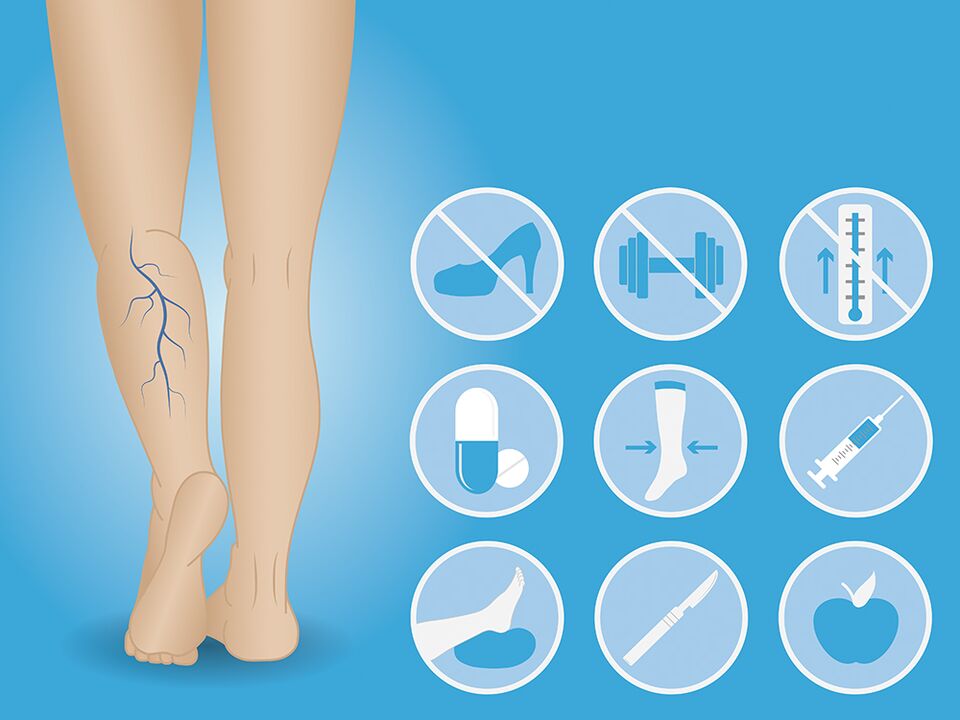
Possible causes of the development of varicose veins in the lower extremities.
- Physical inactivity- the main cause of varicose veins. A sedentary lifestyle and prolonged sitting contribute to a high and prolonged load on the venous valves. During physical activity (walking, running, swimming), constantly working muscles in the thigh and lower leg help to "expel" blood from the venous system of the lower extremities. Static sitting for a long time in a sitting position leads to increased load on the venous valves, and over time, the venous valves, unable to withstand the load, may stop performing their function altogether.
- Obesityshould be considered the second most important reason. High weight also increases the load on the valvular system of the veins of the lower extremities, contributing to the alteration of their correct functioning.
- The pregnancyIt is the third most common cause. Hormonal changes, increased body weight, and compression of the pelvic veins by the fetus are sufficient reasons for venous valve dysfunction. However, up to 50% of changes in the venous wall detected during pregnancy are functional in nature and disappear on their own during the first year after birth.
- Of smoking– the fourth most common cause of varicose veins. Changes in the venous wall may be associated with the unfavorable effect of the composition of smoking mixtures on the tone of the venous wall.
- Inheritance– another possible reason for the development of varicose veins. It is generally accepted that heredity plays a major role in the development of varicose veins, however, the genes responsible for the development of varicose veins have not yet been discovered; It is generally accepted that genes responsible for changes in the structure of connective tissue are the main cause of varicose veins. However, the influence of heredity can be greatly exaggerated, and lifestyle changes, normalization of body weight and quitting smoking will help avoid varicose veins even in patients with an unfavorable hereditary history.
Signs of varicose veins
- Presence of dilated saphenous veins., the non-linear course of the vein is the most objective, but not the only, manifestation of varicose veins. Often, even several times dilated veins may not be visible, especially if they have a pronounced subcutaneous layer.
- Edema of the lower extremities.at the end of the work day, especially in case of asymmetrical swelling, are the earliest and most common sign of varicose veins.
- You should also think about the presence of varicose veins whenpresence of heaviness in the legsin the afternoon and at night, leg cramps at night.
- Spider veins and venous patternIntradermal veins, although more of a cosmetic problem, can also indicate the presence of changes in the saphenous veins.
- Persistent redness, thickening of the skin., lipodermatosclerosis, trophic ulcers on the foot and leg indicate a decompensated course of varicose veins.
Diagnosis of varicose veins.
The diagnosis of varicose veins of the lower extremities can only be made on the basis of ultrasound diagnostic data.
During ultrasound of the veins of the lower extremities, the doctor examines in detail the characteristics of the deep and superficial veins from the groin to the ankle, measuring the diameter of the veins, analyzing the characteristics of blood flow in the veins, and detects the presence of reflux. Based on the data obtained, the doctor reaches a conclusion.
Prevention of varicose veins
Prevention of varicose veins consists of a rational motor regime, normalization of body weight and quitting smoking.
If there are early signs of varicose veins, venotonics and the use of compression stockings will help reduce the rate of disease progression.
Compression stockings should be selected by a doctor based on the severity of varicose veins and the patient's anthropometric data.
Treatment of varicose veins
The treatment of varicose veins is exclusively surgical.
Currently, many different methods of surgical treatment have been developed, from open techniques, combined phlebectomy to minimally invasive methods, laser or radiofrequency vein coagulation, mechanochemical methods.
- Varicose veins can be removed using a miniphlebectomy, a technique in which the varicose veins are removed from the subcutaneous tissue using separate punctures and bandaged.
- Small varicose veins can be eliminated by sclerotherapy - the introduction of a special glue-like substance, sclerosant, into the venous lumens.
- Spider veins and intradermal veins can be removed using sclerotherapy.
However, even after completing treatment, the risk of recurrence of varicose veins of the lower extremities is 10-15%. Adequate physical activity, playing sports (running, walking, stationary cycling, swimming), normalizing body weight and giving up bad habits will help reduce the likelihood of relapse after surgical treatment. Periodic use of phlebotonics and the use of appropriately selected compression stockings will help reduce the rate of spread.
The main thing is not to delay visiting the doctor!

















